
Millions of US citizens suffer from mental health disorders from mild to severe. Mental health sufferers are found in all ages, genders, races socioeconomic statuses, and professions. Healthcare workers are not immune. Yet, despite the staggering numbers, stigmas and lack of knowledge about symptoms and treatments exist. What is the role of the healthcare industry in educating our patients and ourselves about those stigmas and treatment options?

In the United States, it is estimated that one in five adults (57.8 million people) experienced mental health issues in 2021 and 19.4 million adults experienced a concurrent substance use disorder during the same year. 50% of mental illness begins by age 14 and 75% by the age of 24. And even 17% of all youth experience some form of mental health disorder.
Even though there is a staggering amount of mental illness, there continues to be a stigma surrounding treatment. People affected by mental illness continue to interact at work and in life every day without seeking the treatment they need. Mental health treatment -therapy, medication, and even self-care- have made recovery from these conditions a realistic goal, however making the vital first step to ask for help is difficult and confusing for many. It is estimated that only 47.2 % of adults with mental illness received treatment in 2021. There is an average delay between the onset of mental health symptoms and treatment of 11 years. Men are much less likely to seek care than females and people of color are less likely than their white counterparts to seek help.
Stigmas surrounding mental health are a barrier to seeking assistance. Public misconceptions about mental health, and labeling people with mental health conditions lead mental health sufferers to fear social isolation and discrimination. Fear of discrimination in life, employment, education, relationships, and even housing are also barriers to care. People may internalize the negative stereotypes and beliefs leading to reduced self-esteem and reluctance to seek treatment.
Frequently people are unaware that their feelings or actions are symptoms of mental illness. Our society has long been one of resiliency and self-sufficiency. Asking for help goes against those principles and is sometimes viewed as a failure. Those stigmas make it challenging for patients to overcome the stereotypes and seek help. Educating our patients and our healthcare workers about those symptoms brings awareness to the issues so mental health can be discussed and appropriate referrals made before dire situations occur. Healthcare workers need to be educated on assessing for mental illness just as we would assess vital signs. Questions need to be asked without biases and they should be done at every encounter. Patients need to be permitted to ask for assistance if any symptoms arrive so that appropriate help can be arranged.
In addition to assessing for symptoms of mental illness, healthcare workers need to assess for risk of suicide. We need to be comfortable asking questions that assess if a patient is at risk for self-harm and take precautions if those risks are present. Educating the patient and family members on the symptoms may alert someone when they are at risk for suicide. Suicide is the 12th leading cause of death in the US and 90% of those who die by suicide may have experienced mental health conditions according to interviews with their family friends and medical professionals. Educating about the 988 hotlines for suicide prevention is a must for all people. 988 lifelines can be called or texted. and can be contacted by the person thinking of suicide or friends and family of the person. Hotline personnel are trained to help the suicidal person and give support to those who know someone who is struggling with suicidal thoughts. Providing resources and contracting with patients is a must.
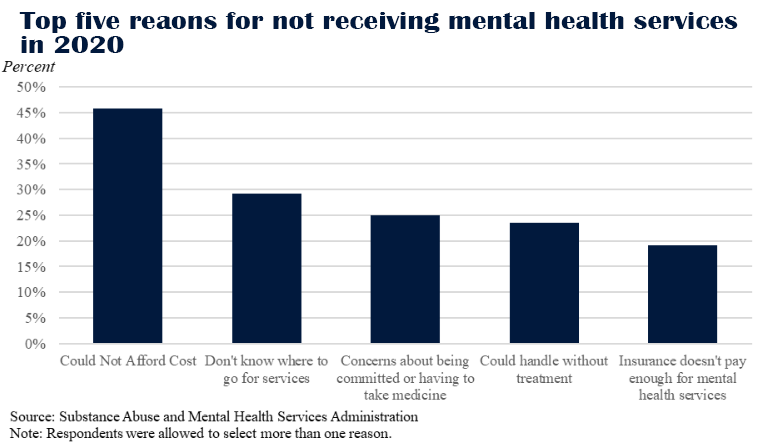
Connecting patients with mental health professionals for ongoing care is a vital part of our care. Unfortunately, there is a shortage of mental health workers in the US. 169 million people live in areas designated as having Mental Health Professional Shortages. Insurance coverage for mental illnesses is frequently paid at a lower rate or not covered at all making care unaffordable.

Healthcare workers are not immune to the risks of suicide, they are at a higher risk for suicide than the general population. The reasons for these higher risks are multifaceted, but some of those risks Reported are:
Nurses and healthcare workers have their own stigmas surrounding their mental health. They have a fear of judgment from other healthcare workers. They hold themselves to a higher standard and feel that they are “called” to serve which implies self-sacrifice of their physical and psychological self that prevents them from seeking treatment. The pandemic increased these issues and in one report taken in June of 2020, up to 30% of healthcare workers surveyed reported they had considered suicide in the past month and 13% reported using alcohol or illicit drugs to manage stress related to the pandemic. Normalizing stress and mental health issues within the healthcare community is necessary to prevent burnout, depression, and even suicide. Educating staff, preparing for stressful situations, debriefing following traumatic events, connecting with employees, and supporting their needs are essential for reducing mental health issues within the healthcare community.
Health.edu provides multiple mental health-related topics for participants to learn how to meet the needs of the patients in the communities we serve and when caring for ourselves. We recognize that mental illness can make it challenging to live everyday lives and make caring for our patients difficult. Education is the key to bridging the gap. The more we know as healthcare workers, the more we can help our patients recognize symptoms and start down the path to healing. As healthcare workers, we can also begin to recognize the symptoms in ourselves, and our coworkers and seek or recommend treatment when needed.